The hype around artificial intelligence in healthcare often paints a utopian picture where advanced algorithms act as a technological silver bullet, ready to cure our most chronic ailments. From streamlining diagnoses to eliminating administrative waste, the promise is a system made radically more efficient and effective. But this vision collides with a stubborn reality: healthcare is a uniquely complex ecosystem, saddled with entrenched incentives, regulatory hurdles, and a deep-seated resistance to change.
While AI tools are being adopted in pockets, the sweeping transformation many predicted has been throttled to a slow, methodical crawl. The central question isn’t whether the technology is powerful, but whether the system is ready for it.
We spoke with Dr. Spencer Dorn, who brings a rare, multi-faceted perspective to this challenge. As the Vice Chair of Medicine at the University of North Carolina at Chapel Hill, a member of his health system's informatics team, and a practicing gastroenterologist, he sits at the precise intersection of clinical practice, high-level administration, and technological implementation. According to Dorn, the reason for the slow pace isn't a single barrier, but the absence of a single, critical ingredient.
For technology to trigger a seismic shift in an industry as resistant as healthcare, it needs a powerful forcing function. Dr. Dorn points to two historical examples: the move to electronic health records, driven by billions of dollars in government incentives through the HITECH Act, and the rapid pivot to telehealth, necessitated by a global pandemic. AI, he argues, is missing that catalyst.
No burning platform: "AI right now lacks a fundamental 'burning platform' to accelerate adoption," Dorn says. Fortunately for the sake of public health, "we don't have billions of dollars in incentive payments or a pandemic that is causing people to be afraid to use healthcare in the absence of AI," thus slowing its adoption due to technological complacency.
One size fits none: The lack of a forcing function is compounded by the sheer complexity of the field. The idea that a single AI tool can be universally applied ignores a fundamental truth. "Healthcare as a concept is not one single thing," Dorn explains. "It is an amalgamation of an infinite number of scenarios, and the notion that we'll just have some magic tool that will apply well across all scenarios is disconnected from reality." This complexity amplifies the natural inertia of large organizations. "Change is hard," he noted. "In healthcare, it's especially hard for very large organizations that tend to be change resistant to move toward new 'bright shiny objects' that carry potential risk."
But this does not mean AI lacks a foothold in healthcare. It is succeeding in specific areas where the risk is low and the value proposition is crystal clear. AI scribes, for example, have seen widespread adoption because they automate documentation (a task many physicians dislike) and the concept was easy to imagine for doctors already familiar with human scribes. The other major area is in back-office administrative tasks like billing and revenue cycle management. As Dorn puts it, "No one will die if one of these tools messes up." So while there is money on the line, human lives are a step removed.in better healthcare outcomes ahead.
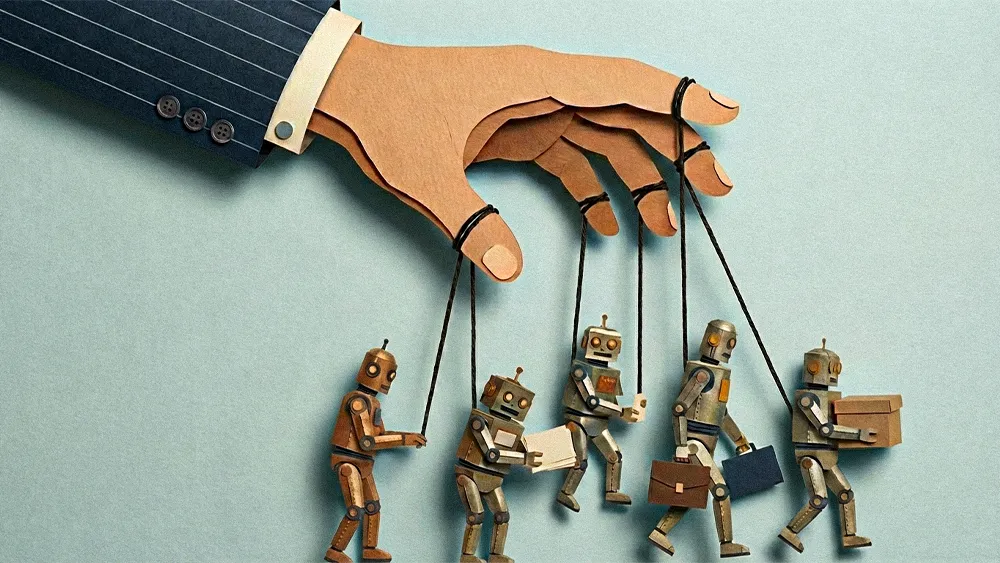
For a healthcare workforce already facing high patient loads and burnout, the promise of AI is that it will reduce their burden. But Dr. Dorn warns of a counterintuitive risk that is rarely discussed. Instead of saving time, implementing imperfect AI could make things worse. "There's a risk that AI makes the work lives of doctors and nurses harder, adding more burden because now we're being forced to supervise a machine that's imperfect and pay attention for errors that may be hard to spot."
A human-centric fix: Ultimately, the path to successful transformation isn't about finding the most advanced tool; it's about focusing on the people it's meant to serve. The core challenge, Dorn argues, is that we often get so lost and enamored with the "super fascinating, magical-appearing technology." But, he stresses, that's beside the point.
Beyond the tech: "It's not about the tech, it's about the people," he says. "It's about the people receiving the care, it's about the people providing the care, it's about the people paying for the care." This requires a fundamental rethinking of care delivery itself.
Reframing the problem: Bolting a tech solution onto a broken process inevitably yields subpar results. Dorn offers a simple example: an AI bot that can perfectly schedule a pediatrician's appointment is useless if the doctor is already booked for months. "Successful AI implementation is not just about the tools, but everything around how they're used. It's really about reframing what we do and how we do it."
For healthcare leaders, the path forward requires a new mindset of holding two opposing ideas at once. "We should be optimistic and excited about AI's long-term potential, but at the same time, we should be skeptical of claims that it will fix things quickly. We need to temper our excitement, keep our feet on the ground, and realize that in many ways, this might be harder than we imagine." The results will undoubtedly speak for themselves, thus making today's work pay off.